Insurance Eligibility Verifications and Pre-Authorizations
Eligibility and insurance verification are critical in the medical billing process. Failure to confirm eligibility and get prior authorization can cause delayed payments and denials, resulting in decreased collections and revenues. Having prompt and accurate determination of the patient’s eligibility provides healthcare providers a clear view of the patient’s coverage, benefits, and payment obligation. With eligibility verification processes, healthcare providers can submit claims effectively & streamline their medical billing process. This also avoids claim resubmission, reduces demographic or eligibility-related rejections and denials, increases upfront collections that lead to overall improved patient satisfaction.
SunTec India is a leading insurance eligibility verification company and has been providing a series of medical billing and coding services to global clients for over 25 years. Leverage SunTec India’s Healthcare’s Eligibility Verification and Pre-authorization services to optimize your revenue cycle and improve collections. We provide insurance verification services that are focused on reducing claim denials and ensuring quick reimbursement.
If you discover that verifying insurance claims is consuming a long time and occupying your staff resources that could be allocated elsewhere, outsourcing your insurance verification services to us can act as an ideal solution. With us, you can leverage the expertise and experience of our medical insurance experts to revamp and strengthen your insurance eligibility verification process in a hassle-free manner.
Pre-Authorization Services
As a part of our Pre-Authorization services, we help you get prior approval for a service from the insurance carrier that results in prompt payment and decreases denials. Our medical billing team obtains the Pre-Authorization on behalf of any healthcare organization thereby easing the burden of your front desk. Our specialists can help you in:
- Contacting the respective care management department for approving pre-authorization.
- Place the request on behalf of the client
- Explain the Medical necessity
- Obtain the Prior authorization within a quick turnaround time
- Report the approved and denied authorization information prior to the patient’s schedule.
Pre-Verification Services
Once the patient is scheduled for an appointment, Insurance Verification is the very first step. This process is the best method to lower the denials from the payer resulting in increased revenue. At SunTec India, we provide real-time validation of patient’s health insurance. As part of our clinical data management services, our highly proficient specialists collaborate diligently with patients, healthcare organizations, and health insurance companies to ascertain the coverage benefits. All information of the patient is verified prior to the service being rendered. The dedicated eligibility verification team validates the patient’s insurance coverage and finds what payment can be expected from the patient and from the insurance companies.
Insurance Eligibility Verification Services we Offer
Our medical BPO team incorporates the most skilled and talented insurance specialists who can cater to Insurance eligibility verifications and pre-authorizations needs. Some of the Pre-certification & Insurance Verification offerings include-
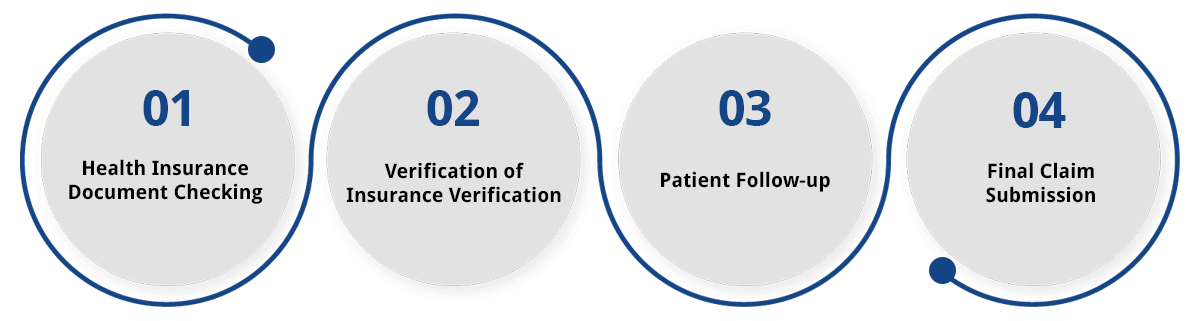
Health Insurance Document Checking
On receiving necessary documents from your healthcare organization, we carefully analyze all the documents & verify them before the scheduled appointment. On checking all the relevant documents, we compile the paperwork & arrange them sequentially as demanded by the insurance company.
Verification of Insurance Verification
Our medical billing experts verify insurance E&B and insurance coverage details with primary & secondary payers. We take necessary details such as co-insurance, copay, deductible, PCP name matching, in-network, and out-of-network benefits, and update these details in the patient notes. Finally, the team completes the verification by either calling the insurance provider directly or by accessing their online portal.
Patient Follow-Up
As a part of our service procedure check, for any incorrect or missing information required our team actively follow-up with the patients and contacts them to correct or fill in any missing details. This enables us to keep track and verify all relevant information & documents before its final submission.
Final Claim Submission
As a part of our final claim submission, we provide our clients with the final results. This includes required documents & relevant information such as member ID, group ID, insurance coverage dates, copayment (co-pay) information, etc.
Insurance Eligibility Verification/ Financial Clearance Process
- We receive patient demographic information from the hospital or clinic or from the patient directly.
- Once the information is received, our team verifies patient information with the insurance company. This includes verification of payable benefits, co-pays, co-insurance, deductibles, claims mailing address, referrals, and pre-authorizations, specific coverage, etc.
- Lastly, we verify if any pre-certification or authorization is required and determine how to connect with the payer to receive the information for updating patient accounts and completing the paperwork.
Pre-Certification Process
As a part of our pre-certification process, our team can enable you to:
- Obtain the pre-certification number needed for a procedure, visit, or other treatments
- Complete or fill appropriate criteria sheets and forms required in the process
- Get in touch with the insurance companies on the physician’s behalf to obtain approval for your authorization request
- Follow up until authorization is received after the forms are filed either online or via a web portal.
- Take further measures or complete documents if necessary.
Outsource Pre-Authorization Services to SunTec India and Step-Up your Billing Process
We at SunTec India understand that you must be reimbursed for the care you provide. By outsourcing your Insurance Eligibility Verifications and Pre-Authorization services to us, you don’t have to worry about this. Our skilled team can help you ramp up your billing process so that you get paid quickly.
As a pre-authorization company, we have been catering to the diverse needs of healthcare organizations with our reliable pre-authorization services. Our team proficiently collects all details regarding procedures and contact payers to obtain pre-authorization quickly. Before submitting the request, our medical billing professionals ensure that payer criteria are met along with all necessary documentation including a letter of medical necessity, payer-specific prior authorization form patient medical records, medical history, and other information specified by the payer.
Outsourcing insurance verification and pre-authorization services to SunTec India, you can benefit in the following ways:
- A higher number of clean claims
- Reduced demographic and eligibility rejections and denials
- Increased upfront collections
- Substantial reduction in operational costs
- No long-term yearly contracts
- Reduced coverage errors
- Improved first pass rate
- Less number of claims re-submission
- Increased self-pay collections
- Improved patient satisfaction
- Optimized cash flow
Business Benefits of Insurance Eligibility Verifications and Pre-Authorizations
Insurance eligibility verification is the first and one of the crucial steps in the overall medical billing and coding process. In many cases, the medical claims are denied or delayed by the insurance companies largely due to incorrect or inadequate coverage details provided by the patients during their visits. Denials can also be a result of incomplete coverage information is by the hospital or administrative staff, resulting in hampering the cash flow of the company by delaying the reimbursements.
At SunTec India, we have been offering quick and efficient eligibility verification services to global clients for over twenty years. Outsourcing Insurance eligibility verifications and pre-authorization services to SunTec India can have you updated with all the regular changes in health plans and policies, and help you prevent delays and denials of insurance claims. Our precise and cost-effective clinical data management services not only help reduce overhead costs but also allow you to allocate your resources more efficiently, enabling you to prioritize and enhance patient care while focusing on core functions. Outsourcing insurance eligibility verification services to us will help you process your medical claims quickly, & improve your cash flow notably.
Discuss your Insurance Eligibility Verifications and Pre-Authorizations Services Requirements with us
- Insurance data security
- Cost-effective solutions
- Use of latest medical billing technology & software
- Quick turnaround time
- Accurate verification services
- Ease of scalability
- Two decades of experience
- Expert medical billing team
Planning to outsource insurance eligibility verification to a reliable service provider, then look no further. Get in touch with us at info@suntecindia.com today!
David Barrs, President
VisionSpan Corporate Communications, Inc., USA